Daniel Rotroff Research Program
-
Daniel Rotroff Research Program
- Principal Investigator
- Research
- Our Team
- Publications
- Careers
- Research News

Daniel Rotroff, PhD
Assistant Staff
Director, Center for Quantitative Metabolic Research
Email: [email protected]
Location: Cleveland Clinic Main Campus
Research
We use a wide-range of computational and experimental approaches to leverage -omics technologies and electronic health records (EHR) to investigate many aspects of precision medicine, such as biomarker or risk allele discovery for drug response and disease outcomes. As a KL2 Scholar, we have funding to develop methods that utilize genomic and clinical data to identify high-risk subtypes within type 2 diabetes. Additional funded projects include the integration of genomic, behavioral, and microbiome factors into a risk model for onset of chemotherapy induced nausea and vomiting, and the use of breath-based metabolomics as a screening tool for chronic liver diseases and hepatocellular carcinoma.
Biography
Daniel Rotroff is Assistant Staff in the Department of Quantitiative Health Sciences and Assistant Professor of Medicine at the Cleveland Clinic Lerner College of Medicine at Case Western Reserve University.
My lab focuses on using computational approaches to investigate and better understand the development and treatment of complex diseases. We use a wide-range of computational and experimental approaches using -omics technologies to investigate many aspects of precision medicine, such as biomarker or risk allele discovery for both drug response and disease outcomes. We have several ongoing projects in the areas of type 2 diabetes, cardiovascular disease, obesity, hepatocellular carcinoma, among others. My graduate work was conducted at the University of North Carolina at Chapel Hill and at the National Center for Computational Toxicology at the US EPA. My postdoctoral work was spent in the Bioinformatics Research Center at North Carolina State University.
Education & Professional Highlights
Research
IDENTIFYING ENDOPHENOTYPES IN COMPLEX DISEASES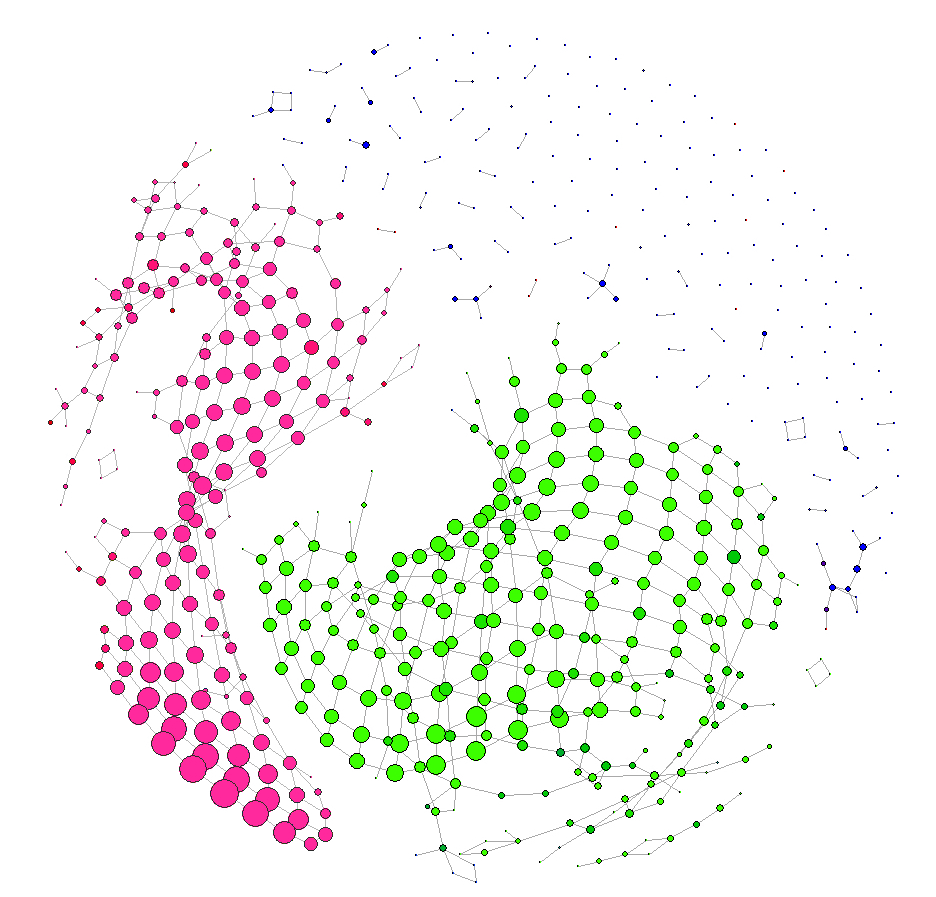
Type 2 Diabetes (T2D) is at record high levels and the incidence is increasing with an estimated 1.4 million new cases diagnosed each year in the United States. Although many drugs are available to treat T2D, the number of subjects that do not respond to therapeutic intervention is too high and T2D is a significant risk factor for cardiovascular diseases (CVD) and mortality. A better understanding of T2D etiology is essential for developing more targeted therapies and preventing the adverse outcomes associated with T2D. Current research suggests that the presentation of T2D is actually a heterogeneous disease with the possibility of many underlying etiologies.
Using a cohort of individuals with T2D in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) clinical trial, we trying to identify subtypes of T2D at greater or reduced risk of CVD related adverse events. This requires developing new methods for identifying subtypes of disases and using the driving features in the construction of new genetic risk scores (GRS) that can predict risks of adverse outcomes.
Aim 1: Identify subtypes of T2D based on clinical features and associate subtypes with adverse outcomes. Hypothesis: T2D is a heterogeneous disease and clinical variables recorded in the ACCORD clinical trial can be used to identify subtypes of T2D capable of explaining variation in treatment outcomes. Approach: We will first cluster individuals based on clinical variables measured at baseline in ACCORD. We will then iteratively group individuals into groups ranging from two to ten groups. For each iteration we will associate individuals in each group with various CVD related adverse outcomes measured in ACCORD to identify groups of individuals at high and low risk.
Aim 2: Identify subtypes of T2D based on SNPs in genes previously associated with T2D and CVD and associate subtypes with adverse outcomes. Hypothesis: SNPs previously identified as being associated with T2D and CVD can be used to identify subtypes of T2D that are at an increased or decreased risk of CVD related adverse outcomes. Approach: First, we will obtain SNPs associated with T2D and CVD in previously published GWAS from the GWAS Catalogue database. Next, we will perform clustering of individuals based on these SNPs and iteratively group individuals into two to ten groups, and associate groups with risk of CVD related adverse outcomes, similar to Aim 1.
Aim 3: Develop genetic risk score (GRS) models for specific adverse outcomes using features enriched in high and low risk subtypes of T2D. Hypothesis: Clinical features and SNPs enriched in subtypes identified in Aim 1 and 2 can be used to develop a more informative and reliable GRS than what is currently available. Approach: Clinical variables in Aim 1 and SNPs in Aim 2 that are enriched in groups with high or low risk of specific CVD related adverse outcomes can serve as strong predictive features. We will use a Cox proportional hazards model within a cross-validation framework to develop a GRS capable of identifying replication cohorts with as features to be selected into a This risk model will be capable of identifying T2D patients at elevated risk of cardiovascular disease related adverse outcomes.
IMPROVING PREDICTION OF CHEMOTHERAPY-INDUCED NAUSEA: INTEGRATING GENES, BEHAVIOR, AND THE MICROBIOME
Chemotherapy-induced nausea (CIN) is one of the most common and feared side effects of cancer treatment despite recent advances in antiemetic medications and international guidelines regarding their use. Approximately 56% of patients treated with moderately- or highly-emetogenic chemotherapy report nausea in the week after their first treatment. CIN is associated with increased hospitalizations and ER visits, greater costs of care, and worse quality of life. Advances in identifying and treating patients at risk of nausea may improve care, reduce costs, and help patients feel better. We believe tailored antiemetic therapy based on patient risk has the potential to reduce nausea. However, more work is needed to improve the accuracy of risk prediction algorithms.
Better risk prediction algorithms may result in superior control of nausea by alerting providers upfront that additional anti-emetics will be needed. Nausea prevention at the first infusion is critical to good nausea control throughout treatment.
The current utility of existing risk prediction algorithms is limited because they are difficult to use or were developed in patients who did not receive highly-emetogenic regimens. In addition, existing algorithms include clinical and personal risk factors (e.g., age, disease site, disease stage, anxiety, alcohol use) but not potential genomic risk factors. Moreover, there have been no studies examining the role of the gut microbiome in the development of nausea. Evaluation of these additional biological factors may improve risk prediction accuracy and suggest new insights about the pathophysiology of nausea. Our study will integrate genomic, clinical, personal, and gut microbiome risk factors for nausea.
We are conducting the first GWAS of CIN, and will develop and validate new risk algorithms based on these factors in patients receiving moderately- or highly-emetogenic chemotherapy. A total of 2,650 patients are being recruited from five cancer centers in the Oncology Research Information Exchange Network (ORIEN), which share a common protocol for data and specimen collection.
Aim 1: To conduct a genome-wide association study of nausea in cancer patients receiving moderately- or highly-emetogenic chemotherapy We hypothesize that genetic variation will be associated with chemotherapy-induced nausea.
Aim 2: To develop and validate a new algorithm to predict clinical risk of nausea based on genomic, clinical, and personal factors including a patient-reported proxy of gut microbiome diversity
Aim 3: To examine associations of the objective gut microbiome with chemotherapy-induced nausea We hypothesize that patients with low microbial diversity before chemotherapy will be more likely to experience nausea. We will create a risk algorithm to explore the independent association of pretreatment microbiome diversity with nausea. We will also characterize changes in microbial diversity from pre- to post-chemotherapy.
WHOLE GENOME PREDICTION OF DISEASE RISK AND DRUG RESPONSE
Although associations with individual genetic variants have been instrumental in advancing our knowledge of disease etiology and in the identification of new drugs, these studies usually only explain a small amount of the overall genetic contribution to a disease. Therefore, developing models that can incorporate genetic information across the entire genome would be expected to do a better job at identifying people at risk of developing a disease or experiencing a side-effect of a new drug.
Available tools exist for doing whole-genome prediction in related populations (e.g., agricultural settings); however, they perform poorly when used on unrelated populations (e.g., human populations) due to the complex correlation structure in the human genome. Convolutional neural networks (CNNs), a form of deep learning, are excellent at learning from data with correlation structures. This is why CNNs are so popular with image recognition -- they identify correlated groups of pixels that can be used as distinguishing features for prediction.
We are exploring the use of these models to identify regions of single nucleotide polymorphisms (SNPs) that are they can be used to construct deep learning models to perform whole genome prediction. If you are interested in this project, please feel free to contact us at the bottom of the home page.
Our Team
Selected Publications
View publications for Daniel Rotroff, PhD
(Disclaimer: This search is powered by PubMed, a service of the U.S. National Library of Medicine. PubMed is a third-party website with no affiliation with Cleveland Clinic.)
Careers
Training at Lerner Research Institute
Our education and training programs offer hands-on experience at one of the nationʼs top hospitals. Travel, publish in high impact journals and collaborate with investigators to solve real-world biomedical research questions.
Learn MoreResearch News

Researchers investigate machine learning models’ ability to analyze electronic health records for patterns in disease development.

Dr. Daniel Rotroff works with physicians to identify and understand biological factors that can help diagnose and manage complex diseases.

The Daniel Rotroff Lab is teaming up with ophthalmologists to identify molecules that predict who will experience relief from eye pain after cataract surgery.

Researchers found that, despite previous reports, blood sugar increases were not significantly different in COVID-19 positive and negative patients.

Dr. Rotroff and team found that genetic variation may help to identify diabetes patients at risk for cardiovascular disease who may benefit from aggressive glycemia treatment.

Dr. Rotroff and clinical collaborator Dr. Foss will compare genetic, epigenetic and metabolomic data from breast cancer patients who experience the condition versus those who don’t in an effort to develop a predictive machine learning-based algorithm for personalized risk.